

To understand the cause of ptosis it is important to review the anatomy of the lid. In facial musculature there are key muscles which function to elevate the eyelid (Tyers, 2018), these include the levator palpebrae superioris (LPS), which is a muscle that originates from the roof of the orbit and fans forwards to fill and insert into the tarsal plate and skin of the eyelid as an aponeurosis (Tyers, 2018). It is the main elevator of the lid (Tyers, 2018) and is innervated by the oculomotor nerve (Tyers, 2018). It has a counterpart known as the Müller's muscle, which is a small muscle attaching to the posterior aspect of LPS and inserts only into the tarsal plate. It is supplied by the sympathetic nervous system and is involved in partial elevation of the upper lid (Snell, 2013). The antagonistic muscles to the elevators are the depressors responsible for closure of the eyelid. This is orbicularis oculi and is innervated by the facial nerve (Bowling, 2016).
Types of ptosis
There are several causes of ptosis (Bowling, 2016). Lifting of the lid is an intricate process and by understanding the pathology the complexity of this function can be fully appreciated.
Neurogenic ptosis
This is caused by pathology affecting the nerve supply to either the Müller's muscle, or LPS (Bowling, 2016). The aforementioned Müller's muscle is supplied by the sympathetic nervous system, which arises from the hypothalamus, travels down the spinal cord to the centre of budge at C8-T2 and then exits to ascend the sympathetic chain within the thoracic cavity. It then goes over the subclavian vessels to join the carotid vessels as it enters the cranium and then travels towards the eye (Bowling, 2016). Any pathology along this route can result in a patient presenting with a mild ptosis, anhidrosis and a constricted pupil (Bowling, 2016). This could include thoracic tumours or vascular aneurysms (Bowling, 2016).
Complete ptosis
This is caused by damage to the oculomotor nerve. This nerve originates from the midbrain. As it exits into the cranium, it is located medial to the posterior communicating artery, which is a common site for PCA aneurysms (Shahzad, 2023). Compression from a ballooning aneurysm can result in a loss of supply to the LPS muscle as well as loss of innervation to extraocular muscles, resulting in an eye which is deviated down and out, with a dilated pupil (Shahzad, 2023). This can be associated with severe headache, indicating a rupture of the aneurysm which is life threatening and requires urgent medical review (Shahzad, 2023).
Myogenic ptosis
This is caused by a myopathy of LPS or an abnormality at the neuromuscular junction caused by conditions such as myasthenia gravis or ocular myopathy (Finsterer, 2003).
Involutional ptosis
Involutional ptosis is the most common cause of ptosis. Due to ageing, laxity is lost in the skin and there is loss of elasticity in the LPS aponeurosis (Pelton, 2022). This results in the disinsertion of the aponeurosis from its attachment in the skin of the eyelid, resulting in a heightened eyelid crease and slow progressive ptosis (Pelton, 2022).
Mechanical ptosis
Mechanical ptosis is caused by a weight pulling the lid down such as lid lesions or from recurrent inflammatory lid conditions (Pelton, 2022).
» Ptosis is an important observation for facial practitioners to recognise, as it can have implications in the decisions made regarding treatment «
Iatrogenic ptosis
There are many iatrogenic causes of ptosis. These include ocular surgery and the use of an eyelid speculum (Bacharach, 2021), this can result in complete disinsertion of the LPS muscle, and the development of ptosis after intraocular surgery (Bacharach, 2021). Other causes include history of contact lens wear, with hard lens wearers developing ptosis sooner in life compared to soft lenses (Bacharach, 2021).
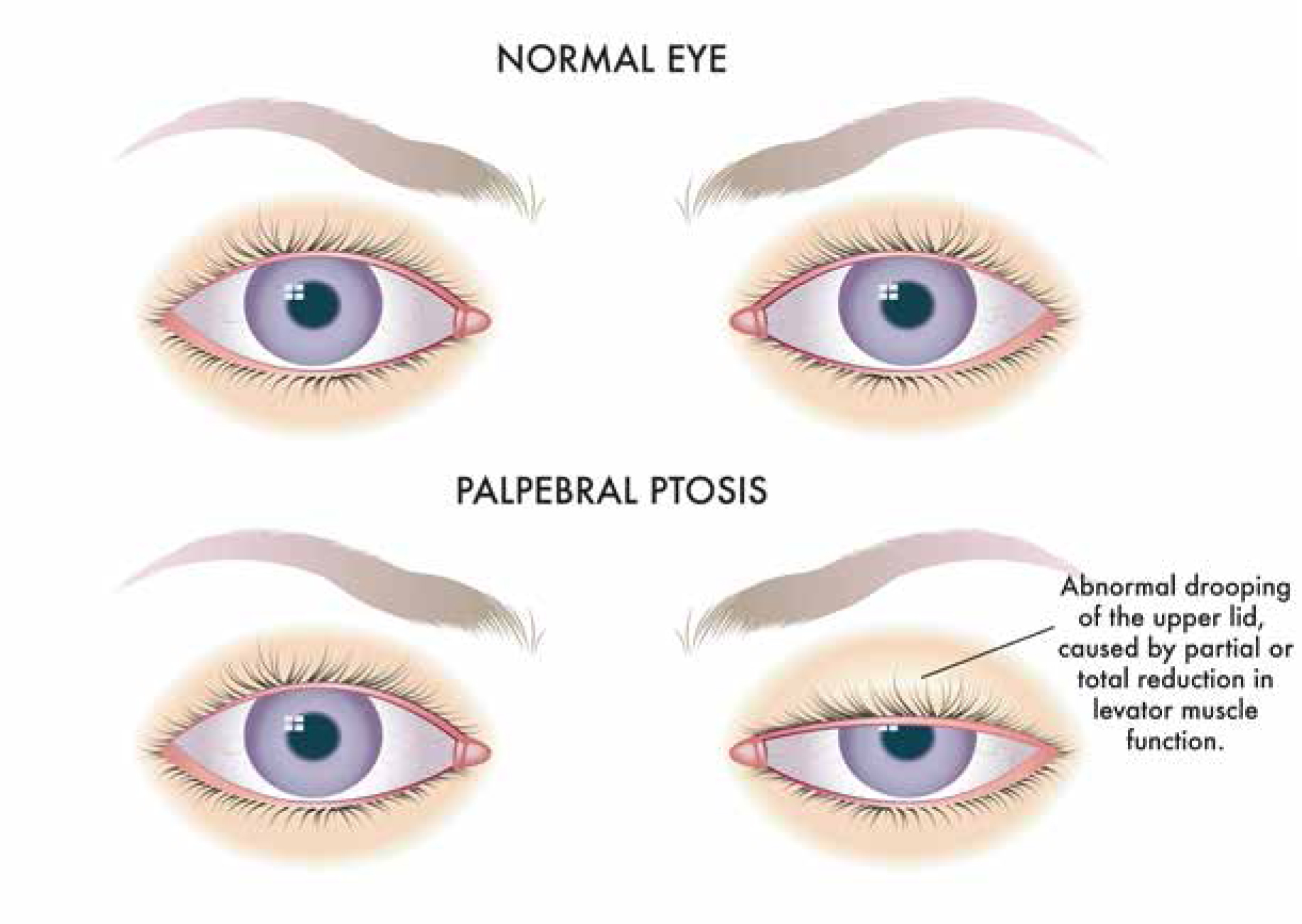
Identification of ptosis
To identify ptosis, as with all examinations it begins with an ‘end of the bed’ evaluation. It is important to assess from the top of the face down.
The examination should begin by looking at the forehead, as there may be frontalis muscle overaction (Wilkins 1982). The cause of this is when the upper lid droops, the frontalis contracts as a compensatory movement which inserts into orbicularis oculi and the skin of the brow (Tyers, 2018). On contraction this elevates the brow and in effect, lifts the lid. Depending on whether the ptosis is bilateral or unilateral, frontalis overaction is evident with rhytides (Wu-Fienberg, 2018).
» In an aesthetic service we have a duty of care to identify possible medical conditions that require medical assessment. Understanding the causes of ptosis can help direct a patient for investigations of other potential causes such as a pancoast tumour or a PCA aneurysm «

The examination should be concluded by moving down the upper face, inspecting the position of the brow. In males they should be located at the superior orbital rim and in females the brow lies above the superior orbital rim, with a lateral arch (Tyers 2018). Their position should be identified and checked for asymmetry. Then, the lids themselves should be examined.
A common misdiagnosis of ptosis is dermatochalasis. This is a condition caused by excess overhanging skin, which can obscure the visual axis and give the appearance of an upper lid droop (Wu-Fienberg, 2018). The key to identifying this is to gently lift away the skin and look at the position of the eyelid margin to rule out a ptotic lid (Wu-Fienberg, 2018).
Examination
If ptosis is identified, it is wise to take photographs and store them in patient notes. If the ptosis is slight, then measurement of the palpebral aperture (distance between the upper and lower eyelid margin in mm) and marginal reflex distance (distance between the central corneal reflex and the upper lid margin in mm, MRD1 and the distance between the central corneal reflex and the lower lid margin in mm, MRD2) can be carried out (Small, 1989).
Why is it important to identify ptosis in aesthetics?
A patient can attend an aesthetic service for treatment of asymmetry. If the ptosis is slight, the cause of asymmetry may not always be identified as the positioning of the upper eyelid. In an aesthetic service we have a duty of care to identify possible medical conditions that require medical assessment. Understanding the causes of ptosis can help direct a patient for investigations of other potential causes such as a pancoast tumour or a PCA aneurysm.
From a practical perspective, if a patient attends the service for treatment of forehead rhytids, a ptosis assessment is important. There is frontalis overaction for ptosis correction and the frontalis muscle is commonly treated with Botulinum toxin A (Finsterer, 2003). If this is the case, this can partially paralyse the compensatory action and cause the ptosis to worsen or become more apparent. If the ptosis covers the central visual axis, the patient is not able to see out of the affected eye until the toxin has worn off. This is a different cause to Botox-induced ptosis and instead related to a shift in the toxin which can affect the mullers muscle. The treatment for this variety of ptosis is topical apraclonidine (Nestor, 2021), which is sympathomimetic. This topical treatment will not make a difference to the brow induced ptosis that toxin treatment to the compensatory frontalis muscle would cause (Nestor, 2021).
Identifying ptosis is also important in surgical planning for both blepharoplasty and other brow related procedures (Leone, 1988).
Conclusion
In conclusion, ptosis is an identifiable condition with many potential causes. A full breadth of knowledge regarding the causes of ptosis accompanied by a basic eyelid assessment, the findings can potentially change a patient's outcome both medically and aesthetically. The identification of ptosis can also have practical implications in regards to how patients are treated with toxins, and the approach to asymmetry. If ptosis is identified, it warrants a referral for an opinion from an oculoplastic surgeon for further investigation and potential treatment.
Key Points
- Neurogenic ptosis is caused by pathology affecting the nerve supply to either the Müller's muscle or LPS
- Complete ptosis is caused by damage to the oculomotor nerve
- Myogenic ptosis is caused by a myopathy of LPS or an abnormality at the neuromuscular junction
- Involutional ptosis is caused by loss of elasticity in the LPS aponeurosis
- Mechanical ptosis is caused by a weight pulling the lid down
- Iatrogenic ptosis has many causes including ocular surgery, use of an eyelid speculum.
CPD reflective questions
- Why is it important to identify ptosis?
- What are the implications of ptosis?
- Do you know how to identify it?



