
The lips and lower face are highly dynamic and complex facial areas which vary greatly between individuals. As a result, there is no ‘one size fits all’ treatment protocol that can provide harmony to this area. We do indeed use concepts of proportions and ratios to approximate aesthetically pleasing targets for treatment, however idealising proportions alone does not necessarily result in ideal enhancement and does not consider distortion of features on dynamism (Farkas et al, 1985). To truly harmonise facial features and provide natural results, careful assessment of both the static and dynamic facial presentation is required (Trévidic et al, 2022). This case study explores the assessment, planning and treatment of lower face disharmony with a focus on correction of misplaced filler in the lips and lower face.
Patient history
A young woman in her 20s attended as she was originally concerned about the appearance of her under eyes. She felt they looked dark and sunken. She had never had this area treated; however she had previously had lip filler a year prior with a medical professional. Medically, she was fit and well with no known allergies. Her only prior aesthetic treatments had been 1ml lip filler and 1ml chin filler over a year ago.
Clinical assessment
On examination, she presented with hereditary tear trough (TT) defects bilaterally, combined with thin, translucent lower eyelid skin. This resulted in a mild sunken appearance as well as darkness from orbicularis oculi (o. oculi) muscle shine through. She was lacking support in the medial cheek but had excellent lateral cheek contour and volume. She had a deep labiomental crease creating a ‘separate’ looking perioral region and migrated lip filler to her upper cutaneous lip bilaterally causing a long philtrum, upper lip inversion frontally and protrusion in profile. There was a heavy appearance to her white roll and a steep lip to chin angle.
Before discussing my findings with her, I had to decide whether to detail my assessment of her lower face. As she had expressed that she was happy with her lower face treatments, and they did not form part of her presenting complaint, I opted not to detail my critique of her existing treatments as it was essentially unsolicited criticism. As facial aesthetics treatments are elective medical procedures, and she was not suffering with any emotional, psychological, or physical problems because of her previous treatment, I did not believe it would be in her best interest to discuss these findings. My discussion with her during her first visit therefore only covered my findings relevant to her presenting concern; her tear troughs. I recommended addition of volume to the cheek primarily, to improve the light reflection across the periorbital and zygomatic regions and provide better support for the delicate under eyes. I advised if there was still a reasonable TT defect after the midface filler had settled, we could fill the remaining defect directly.

Midface & undereye treatment
Her cheek augmentation was performed using a needle technique, depositing a total of 1.2 ml Teosyal Puresense Ultradeep in supraperiosteal boluses, using the proprietary 25G 1″ needle. I targeted the medial SOOF primarily to indirectly soften the appearance of the lid cheek junction. I also targeted the lateral SOOF to subtly enhance the midface light reflection, thereby reducing the emphasis on her under eye shadow.

Four weeks later she attended for review. She was very pleased with the improvement, however there was still a mild TT defect remaining bilaterally. Using a 38 mm 25G cannula, 0.3 ml Teosyal Redensity 2 was administered per side. All filler was deposited in the supraperiosteal layer with linear threads and microdroplet technique. The TT ligament was also gently subcised with the cannula in a deep and superficial plane to help reduce the pull on the delicate infraorbital skin to the bone. The result was a marked softening of the infraorbital volume defect and a much-improved light reflection bilaterally, which reduced the purple hue she disliked.

Lower face disharmony
At her 4-week review, her midface and TT region looked optimal, however her lower face appeared more elongated and angular than at prior visits. Her chin looked pointed and distinctly separate from the surrounding lower face. On questioning her about the visual change, she explained that she had further chin augmentation dermal filler treatment whilst visiting her family home, with her previous practitioner who was local to them. She admitted that she was not completely happy with it and was afraid her chin looked too sharp, not giving the desired effect she had hoped for.
On examination, I could appreciate that her facial thirds were now more proportional, however the contour to the chin appeared to be enhanced purely by deep deposition of filler under her mentalis muscle. This is a commonly used approach for chin augmentation however in this case it caused over prominence of the chin (Beer et al, 2021). This contributed to an overall appearance of more segmented facial features. On explaining my findings, she could understand why she felt these results were suboptimal. I explained that the previous treatment was not ‘bad’ but only addressed one aspect of lower face contour, and this treatment could be adapted to better resolve her lower face disharmony. I recommended that we could soften the pointed appearance by partial dissolving with hyaluronidase injections, and then review with a view to lower face contouring in a superficial plane. This would allow improvement of lower face light reflection and more natural topological transition between facial features (Carruthers et al, 2021).
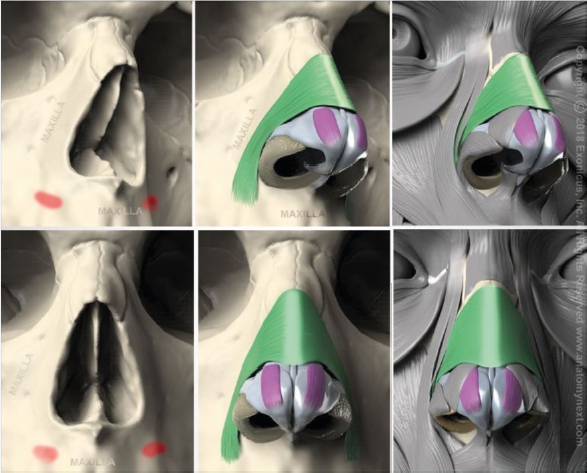
She also asked if I believed she should have more lip filler as she felt her lips were looking smaller recently. I used this opportunity to discuss her lip filler migration and explain that despite having 1ml of filler a year ago, it was still present but made her lips look smaller due to migrating from the pink body to the white roll. This results in more weight in the cutaneous lip which can push down on the pink lip and invert it, thereby reducing the upper lip vertical height whilst exaggerating the lateral projection. Furthermore, it caused excess weight on the lower lip, causing a deeper labiomental crease. She also had a very complex lip type comprised of an M-shaped lip with high muscle tone in orbicularis oris (o. oris) and a naturally distinctive white roll. On smiling and speech, she also contracted her nasalis muscles, which appeared to have a lower than usual point of origin in the incisive fossa. This combination of muscle tone created tension and rigidity in her upper cutaneous lip on function.
I recommended that she did not have any further lip augmentation and instead may benefit from dissolving filler. This could be approached in 2 ways: a) by total dissolving with hyaluronidase injections to the cutaneous migration and upper and lower lips, or b) partial dissolving, whereby only the migrated filler would be targeted with topical hyaluronidase (Topilase). The benefit to the latter approach would be that it would be diagnostic in confirming that the cutaneous filler migration is responsible for the inversion and weight of her upper lip as eversion and lifting should be evident quickly post treatment in this case. Additionally, we may preserve some of her lip filler volume within the pink body, whilst noninvasively improving the contours and proportions of her cutaneous lip. I advised her it was possible we would need injectable hyalase if we did not see significant improvement from topical treatment. She opted to partially dissolve her chin with hyaluronidase injections and partially dissolve her migrated upper cutaneous lip filler topically with Topilase.
Injectable hyaluronidase dissolving technique
LMX cream was applied to her chin and left for 5 minutes, and subsequently her skin was disinfected with Clinisept solution. I did not administer a patch test as literature suggests poor sensitivity of intradermal patch testing, with no validated test concentration of hyalase (Murray et al, 2021). If she had a history of wasp/bee sting allergies, I would have referred her to a specialist allergy testing clinic prior to any dissolving.
Then 1500IU hyaluronidase was reconstituted with 5ml 0.9% bacteriostatic saline immediately before administering 2 deep supraperiosteal boluses at menton and gonion points with a 25G 1″ needle technique. Total 600IU was delivered and then vigorously massaged. In a downwards direction to encourage dissolving of the filler which was causing the elongated facial appearance.
Topilase mode of action
This mix of hyalase, lipase and protease together provide superficial absorption capable of dissolving and remodelling hyaluronic acid (HA) in superficial subcutaneous and intradermal layers. The other natural ingredients including myrrh, citrus, lavender, aloe vera and helichrysum essential oils have a soothing antiinflammatory effect which reduce the appearance of peri or post operative redness or swelling. The more crosslinked, longer present, or deeper placed the HA gel within the tissue, the less effect Topilase may have on breaking down the HA (Kim et al, 2o11). For this reason, Topilase is ideally used either perioperatively during lip filler or tear trough filler treatments for softening the inflamed appearance of the filler site, or for managing instantly visible lumps or Tyndall effect.
Topilase application technique
The Topilase ingredients are activated by pressing the lid and shaking vigorously to mix the components (SoftFil, 2023). Following this, three drops of the solution were applied directly to the cutaneous lip and vigorously massaged with gloved hands. The massage both increases absorption of the solution as well as mechanically breaks down the filler which is being softened by the solution. Immediate mild erythema is normal due to the massage, however, should settle quickly. Immediately after application, the upper cutaneous lip contour improved with a natural upper lip eversion restored and shorter philtrum length noted.
Post operative care instructions were given and it was recommended to return for review with a view to retreatment of the lower face as required, after a twoweek interval.
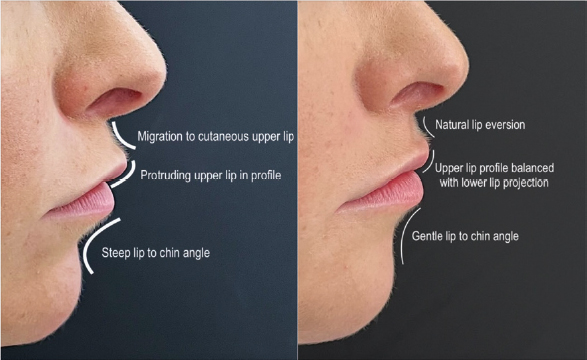
After two weeks, the patient presented for reassessment. Her pointed chin appearance had softened however she appeared slightly retrognathic in profile. Her prejowl sulcus shadows looked less prominent bilaterally but she still had a defined labiomental shadow. Her upper lip had everted well and now had more ‘pink show’ than prior to dissolving, with a more natural upper cutaneous lip convex profile. We agreed on treatments to optimise her proportions, myomodulate her lateral nasalis muscles and provide better topological transition between facial features (de Maio, 2020; Kane, 2018). 0.3 ml Teosyal RHA4 was deposited per side with a 25G 1″ needle in the supraperiosteal layer of the pyriform space, and 0.1ml fanned superficially per side with 25G 38 mm cannula at the crest of the nasolabial folds. By sandwiching the nasalis at its origin between strong but flexible filler, the muscle may lengthen and the action of nasalis could be subtly reduced whilst maintaining natural topological contours. I opted against treatment with botulinum toxin at the nasalis origin as it was possible to get better longevity treatment outcome with filler that may alter the causative muscle action. I could also avoid inadvertently affecting levator labii superioris alequae nasii (LSAN) movement that could give her an undesirable longer upper cutaneous lip.
Her chin, prejowl and labiomental crease were treated with a multilayering approach. 0.1 ml RHA4 was deposited by needle as supraperiosteal boluses in the prejowls, followed by a total 0.3 ml subcutaneous fanning with cannula to labiomental crease and inferior mandibular border between the prejowl and menton.

Results
The overall result was a natural looking, subtle enhancement, with smooth transitions between the perioral, chin and jawline areas. Natural profile contours were restored to the upper cutaneous lip and the lip to chin angle, resulting in less shadows being cast on her lower face. Her static proportions were balanced whilst respecting her dynamic anatomy.
Key points
- Facial assessment should include careful observation of musculature, light reflection and shadows, to help optimally beautify patients and prevent potential filler migration and unnatural contours
- The use of Topilase should be considered as a minimally invasive treatment option, when aiming to improve the appearance of superficial migration of soft HA fillers, particularly in the perioral region
- Injectable hyalase is still the treatment of choice when aiming to remove or reduce the appearance of deeply placed, or highly crosslinked HA fillers
- Multilayering fillers in dynamic areas with suitably cohesive or flexible fillers will give optimal visual results
- Consider myomodulating muscle activity with HA fillers rather than treating with neurotoxin where appropriate.



