
The rise in popularity for aesthetic treatments has grown significantly in the last decade and this trend looks set to continue (Dodds, 2016), as has the amount of non-medically trained injectors who have discovered that it is not against the law to carry out cosmetic injectables, and thus teach others these treatments with no statutory body overseeing them, with no regard for public safety, even though they have no medical background and often lack extensive accredited training. However, it cannot be ignored that being a medical professional does not make one competent or safe and, unfortunately, there are also some very unscrupulous medical injectors in the aesthetics industry. Although they are answerable to a governing body, with codes of conduct to adhere to, the Joint Council for Cosmetic Practitioners (JCCP) has been implemented by the Department of Health and Social Care to introduce some guidance and frameworks for safety and support (JCCP, 2019).
It raises the question of what this lack of medical training does to the reputation of the aesthetics industry and how standards can be raised to improve the industry and its current state.
Lack of regulation in the industry and steps practitioners can take
This lack of regulation makes the aesthetics industry open to any person to inject wrinkle relaxants and soft tissue fillers at present with no medical training, no evidence of anatomy knowledge, no competency frameworks, no auditing and, most of all, no inspections of products, clinics, practice, health or safety. Staggeringly, this means anyone can order these products from unregulated, non-Care Quality Commission registered suppliers on the Internet who cannot always guarantee the authenticity of the products and could be counterfeit. Unfortunately, a small handful of medical professionals also add to this problem by prescribing and delegating injection tasks to non-medically trained persons, with little or no oversight of supervision to ensure patient safety and desired outcomes are met for the patient.
As a collective group of specialist medical aesthetic clinicians, the following steps can be taken to help with these issues:
- Be medical, ethical, accountable, practice professionally and know your anatomy. The more a practitioner knows, the more cautious they can be and the safer it is for patients. Ensure that JCCP and Advertising Standards Agency guidelines are adhered to, not forgetting statutory bodies and code of conduct
- Train according to the JCCP Matrix, train for a qualification to show ongoing and extensive training, rather than 1 day courses here and there—they are foundation courses for a reason. They are the beginning of a specialist journey, not the beginning and end. This will give providers continuity, as well as support to develop into an aesthetics specialist much more quickly and ultimately make a safer practitioner. This will set injectors above the majority of the industry.
 To be an effective practitioner and give a desired result when injecting botulinum toxin A, it must not just be known where the muscles are, but injectors also need to know how to assess dynamic movement and anatomical landmarks
To be an effective practitioner and give a desired result when injecting botulinum toxin A, it must not just be known where the muscles are, but injectors also need to know how to assess dynamic movement and anatomical landmarks
Injectors with a high level of knowledge in anatomy and physiology in aesthetic medicine have a reported lower rate of complications or adverse events. Knowing more about anatomy and having hands-on clinical experience helps with:
- Being able to support medical colleagues
- Educating patients in safe aesthetic practice and the reasons behind this
- Reducing common side effects: swelling, bruising, discomfort, bleeding
- Reducing rare but possible complications, such as vascular occlusion and anaphylaxis
- Reduces pain/discomfort
- Reassures patients psychologically
- Gives practitioners measurable competence against standards, resulting in confidence.
Understanding anatomy
As is the same in any medical speciality, to treat safely and effectively and reduce risks and complications, it must first be understood not just what and where is injected, but how, with what and why (Harley Academy, 2020).
To do this, it needs to not just be known that some areas are higher risk to inject botulinum toxin A and soft tissue filler than others, but why and how these common side effects and complications can reduce or avoided.
Knowing the body's anatomy and constantly updating one's knowledge by attending accredited and CPD training is fundamental, but not the only factor that must be considered and included in practices.
Let's look at pre-care—for example, no alcohol, NSAIDS, exercise, sauna, skin treatments and so forth is recommended for at least 24–48 hours before facial cosmetic injections, but why? What affect does this have on patients and their treatments?
Vasodilation results in the increased risk of bleeding, bruising and swelling as common side effects. By knowing how the aforementioned activities or any prescribed medications may affect the body and face, preventative measures can be put in place to reduce them.
The same can be said for post-procedure facial injections. To recommend this care, it must be understood how the body works and what is being affected when injecting botulinum toxin A and fillers.
» Without X-ray vision, it cannot be confirmed that a patient has similar anatomy to that of the majority of the population, as evidenced in textbooks. Instead, injectors should learn what they can with the scientific evidence base they have to be the best they can «
As an injector, knowledge of the anatomy gives many benefits. If practitioners are aware of something, they are generally more cautious and will consider alternatives, including every risk versus benefit at each junction of decision-making.
For example, aspirating is an interesting subject to discuss. The technique varies from clinician to clinician. Think about the force when personally withdrawing the syringe plunger, the depth, the speed and by how much. Hand steadiness can affect aspiration even by the slightest millimetre, is there less risk if placing a supraperiosteal bolus compared to retrograding product when withdrawing as practitioners inject through the layers?
Because every injector is different, one injector may aspirate positively in an area and another may not. Techniques with minimal evidence cannot be relied on, the same as textbook anatomy as vessels are movable and not fixed. They move with the dynamic movement of the face and size changes with intrinsic and extrinsic factors. This is why injectors need to be educated enough to have a multiple layered approach to make them safe injectors to the public and able to reduce complications (Teoxane, 2020).
Safety first
Injecting small amounts in multiple layers and areas is said to give more natural results and be safer, as the smaller the amount of product placed in a specific area means reduced side effects like, for example, swelling or vessel, nerve or lymphatic compression. However, if not using a cannula, this could induce more risk of infection with regard to multiple needle entries breaking the skin layers and barriers—not forgetting reduced product longevity.
Without X-ray vision, it cannot be confirmed that a patient has similar anatomy to that of the majority of the population, as evidenced in textbooks. Instead, injectors should learn what they can with the scientific evidence base they have to be the best they can. A multifactorial approach needs to be completed, which always starts with knowing anatomy.
Thorough consultation and assessment
Taking a detailed past medical history, with all medications, including over-the-counter, herbal and prescribed drugs for all routes (oral, topical, IM and IV) and how they affect the face and bodily systems (for example, nerve, circulatory and lymphatic) is necessary. Skincare products and regime, previous facial surgery changing the anatomical structures or any recent surgery resulting in possible immunosuppression and higher risk of infections should also be noted. Patients should also be asked about anticoagulant medications, facial fractures or trauma, whether they smoke, their alcohol consumption, activities and hobbies, especially those affecting the face. This should be followed by a full facial assessment, highlighting any concerns pre-treatment and any possible anatomical asymmetries. Furthermore, issues like atrophy have a predominantly genetic trait and patients may have concerns that arise from volume redistribution, loss and bony reabsorption from the ageing processes.
Multiple approaches to learning about anatomy should be experienced, including cadaver dissections, complications training, self-directed anatomy and physiology to name a few. The more that is learnt, the more the practitioner will be able to understand, and everyone has different learning styles.
Injecting botulinum toxin A
Let's look at anti-wrinkle injecting and botulinium toxin A. So as to inject the correct muscle, we must first know where they are and how to assess their movement, size and strength. Picture and cadaver training is helpful, but every patient is different and ethnicity will also play a huge part here. Furthermore, the differences between the male and the female muscles and anatomy must not be forgotten.
To be an effective practitioner and give a desired result, it must not just be known where the muscles are, but injectors also need to know how to assess dynamic movement and anatomical landmarks. They must also know how deep and in which layer the muscle sits—this again comes back to knowing muscle sizes and features. Each wrinkle injection is given at different depths and in varying amounts. Knowledge of the face's anatomy will help injectors to not only assess more accurately, but to treat more effectively by being able to reduce complications and side effects. For example, this includes being able to assess how certain factors make some individuals higher risk for ptosis. Gender, age, hormonal status, facial proportions, elevator depressor complex, muscle size and strength and previous ptosis experience should be taken into account.
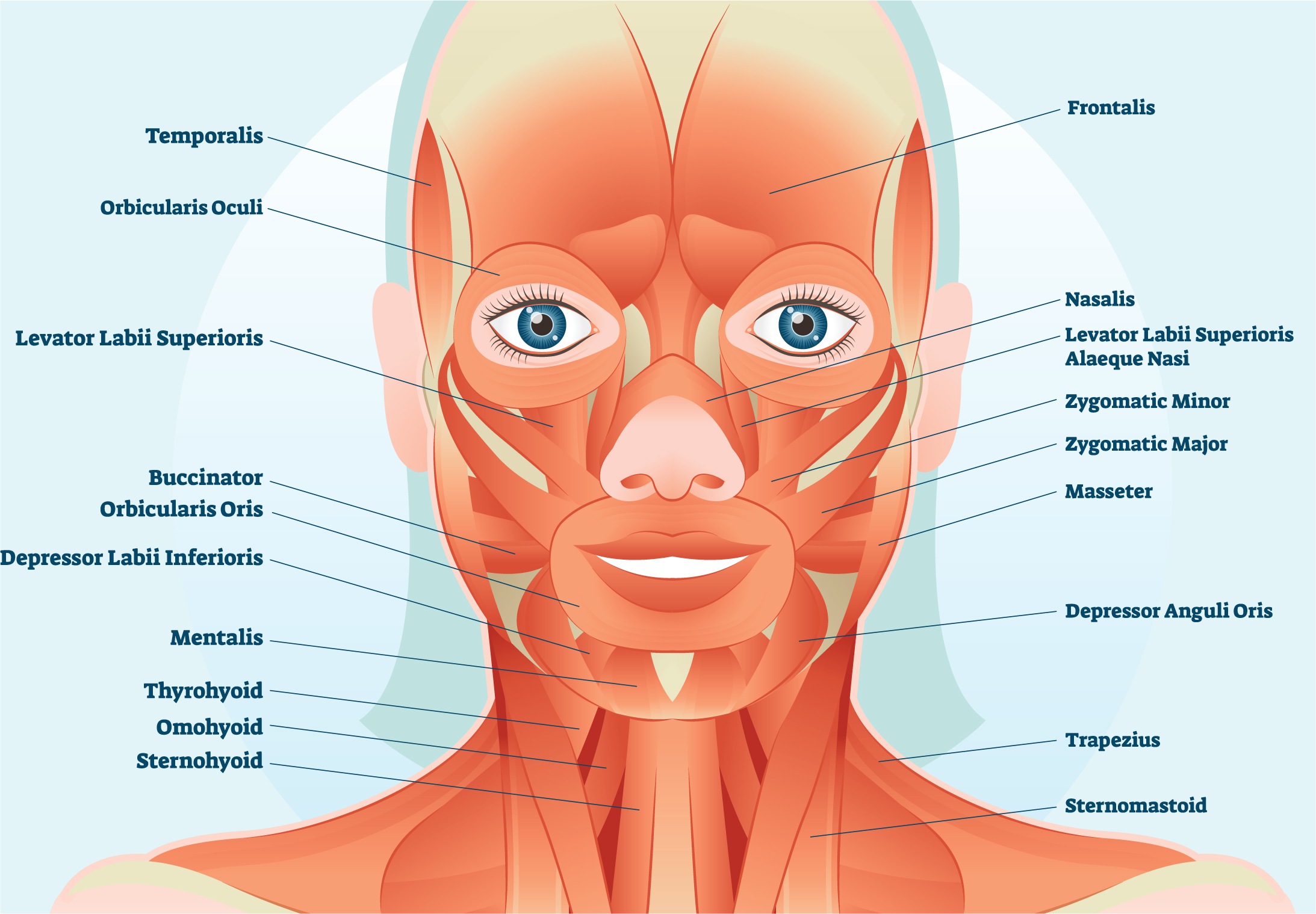 Muscle size needs to be taken into account when injecting the face, as well as how deep and in which layer they sit. For example, the orbicularis oculi is a flat, circular muscle, so injections should be placed 1 cm away from the orbital rim
Muscle size needs to be taken into account when injecting the face, as well as how deep and in which layer they sit. For example, the orbicularis oculi is a flat, circular muscle, so injections should be placed 1 cm away from the orbital rim
For example, the orbicularis oculi muscle is 3 cm in diameter and is a flat, circular muscle, so injections should be placed away from the eye, 1 cm from the orbital rim, superficially. Inject too deeply, and under this muscle are the smile muscles. Inject too deeply here, and the targeted muscle may not be treated and the patient may return with a droopy smile.
Let's look at spocking and ptosis again. To treat effectively, the frontalis muscle does not want to be injected too laterally past the temporal fusion line, missing the lateral movement of the frontalis muscle or have the injections too medial, as both can result in the spock effect.
With ptosis, the frontalis muscle lies underneath the glabella, and if injected too deeply and not along the muscle fibres at the recommended angle and depth, the medial or lateral corrugators may be missed, resulting in a brow or lid ptosis.
» Delayed vascular occlusion gives a false sense of security and urgent reversal is required. Knowing the pathway of the vessels can determine the severity if the practitioner believes the patient has a vascular occlusion and can alter the treatment plan and timing «
Knowledge of drug specifications is also important, and understanding the diffusion of botulinum toxin A in the muscle to be 1–1.5 cm again helps injectors to mark anatomically for the safest effective results, and ensures even distribution and diffusion as much as possible.
With fillers, practitioners cannot just guess which layer they are in. They all feel different. For example, in lips, the majority of people have their artery sat below the muscle, so it is said to inject superficially in layers 1 and 2, which will increase product longevity and reduce the risk of vascular occlusion.
However, there is a percentage of people whose labial artery sits above the muscle. This can be recognised through physical assessment, visually looking and feeling and ensuring good lighting to help with this. However, knowing the arteries and their pathway up to the supratrochlear artery means if injectors do have concerns that they had occluded this vessel, as it is a higher risk area, they would need to act promptly and dissolve following Ace protocols and seeking senior/advanced support if required.
Trauma or surgery
Trauma or surgery alters anatomy. However, no two faces are the same, anyway. For example, the author has injected hundreds of piriform fossas with needles, aspirated and had a positive aspirate. It is recognised that this is a high-risk area, because of the main facial artery, but, anatomically, by the alar, it is said to be superficial but deep on the jaw, so varies in layers of the face and is moveable and variable in size with vessel dilation and constriction. So, if an injector only follows their anatomy knowledge in the maxilla area, are they safe? If a practitioner feels they are on periosteum with their needle and have a positive aspirate, can they inject, as anatomical evidence suggests the majority of the arteries are not in that layer?
Further questions should be asked:
If I only aspirate in this area prior to injection am I safe?
If I use a needle am I safe because I can aspirate?
If I get a negative aspirate does that mean I cannot get a delayed vascular occlusion?
If I only use a supraperiosteal bolus and not a retrograde linear thread am I safe? I am not moving my chosen equipment through multiple facial layers possibly coming into contact with many nerves, lympth glands, arteries and vessels?
If I use a cannula and can be sure I am in layer 5 on periosteum am I safe?
Can I use any cannula to reduce the risk of vascular occlusion?
In the author's opinion, if only one of the factors is considered and used, then no. However, if all the knowledge is applied and put in to practice, risk versus benefit, anatomy known, patient assessed, the correct equipment chosen, correct product, correct layer and treatment, this could mean yes for one patient, maybe. However, it will not be the same for every patient. Injectors need to be able to assess holistically and systematically with factual evidence using evidence-based decision-making for every person and treatment—the same as any other medical procedure.
Anatomy and facial layers
Injectors must start with anatomy, because if not, they are not able to pick the right product. When thinking in layers, remember that highly crosslinked products with large hyaluronic acid molecules and good longevity on periosteum are used. This is not only to mimic and restore bone structure, but because arteries are rarely deep in the facial planes and become more superficial as injected more medially. Injecting this type of product into superficial facial layers will absorb too much water due to its hydrophilic nature and appear strange in appearance with increased swelling, complications, lymph drainage and pressure on vessels, arteries and nerves.
Softer products are used more superficially, not only for dynamic movement and natural appearance, but due to the cohesity of the products and their hydrophilic nature that can occlude superficial vessels that will then penetrate more deeply—hence the filler blindness risk.
The science behind products
Knowing anatomy and which areas are said to be higher risk can enable injectors to use the correct equipment and reduce this (i.e. needle or cannula).
Injectors need to be able to decide on the correct technique and approach of injection (retrograde linear thread, anterior grade linear thread, supraperiosteal bolus, bolus, fanning, and so on).
It is necessary for practitioners to understand the science of their selected products, how they are crosslinked, how they integrate, possible concerns, what approval, research and longevity is evidenced and how and to what extent. Deep insight of each area anatomically and regular injecting before progressing to higher risk areas ensures a higher awareness of all anatomy and layers. Furthermore, regular good injection technique will help placement and experience.
The safety behind anatomy knowledge
Anatomy knowledge will help injectors understand what they want to avoid and why—for example, with what size needle for botulinum toxin A injections. The smaller the needle the better, and, generally, more expensive is less painful for patients, resulting in a more pleasurable treatment.
Cannula use in higher risk areas reduce the risk of vascular occlusion as they have blunt rounded tips, which are less likely to penetrate arteries or vessels and injure nerves or lympthatics. Evidence states that 25 g cannulas are most suitable. Aspiration has minimal to no official evidence base, as aspiration technique is so variable from practitioner to practitioner, with cannula use preferred where possible. This cannot be relied upon, and it is about having a safe approach and understanding anatomy and how to deal with complications. The majority of vascular occlusion cases have been reported to have had preventative care of negative aspiration and still resulted in this.
Delayed vascular occlusion gives a false sense of security and urgent reversal is required. Knowing the pathway of the vessels can determine the severity if the practitioner believes the patient has a vascular occlusion and can alter the treatment plan and timing. Referral plans are an expected safety measure to have in place should the need arise.
Knowledge of anatomy helps both the practitioner and the patient understand why things happen; there is a valid reason for most things. For example, when injecting the lips, it is more uncomfortable than most other facials areas as there are more nerve endings periorally and superficially where practitioners inject the product. The layers are small and have little space to be stretched. This is what medical injectors should be able to educate their patients with and reassure them that they have studied thoroughly for their safety and benefit. Explaining the discomfort that they may be experiencing is short-term and not unexpected and how best it will be managed increases the patient's confidence in the injector. In turn, this reduces anxiety, pulse rate, blood pressure and irritable behaviour, which can increase cortisol levels, swelling, pain and complications if not. Furthermore, the fight or flight response can increase bleeding, bruising and swelling.
Summary
So, in short, knowing layers, depth, product anatomy and many other factors helps the injector to treat, practise safely and choose the right equipment (i.e. cannula, needle or both). It is also imperative to know when to decline treatment, including when the patient is not medically suitable or concerns of body dysmorphic disorder or an otherwise uncontrolled psychological state. Anatomy is fundamental and injectors must understand this, but in a multi-layered approach consisting of many factors. Just one system and method cannot be relied upon.
Key points
- Anatomy is important and fundamental, but not the only factor to be considered in facial injections
- Self-directed learning and adequate certified and verified training is fundamental for patient safety
- Injecting is a scientific evidence-based practice, not guess work.
CPD reflective questions
- Do you know what affects your anatomy, how and why?
- Can you physically assess the ageing process for restoration and rejuvenation, also differentiating between these treatments compared to beautification ones?
- How do you know you are using the right equipment and products and why?



